Does Menopause Cause Urinary Incontinence?
Menopause marks a significant transition in a woman’s life, with its array of symptoms often leading to questions about their origin. Among these symptoms, urinary incontinence can be particularly frustrating, leaving women to wonder if menopause causes urinary incontinence. Let’s delve into the connection between menopause and urinary incontinence, debunking myths and offering practical solutions for managing and alleviating your symptoms.
Understanding Menopause and Its Symptoms
The average age for a woman to experience menopausal symptoms is 47.5 years old,
with menopause typically occurring around age 51. Menopause is defined as the 12
consecutive months without your period, decline in ovarian function, and a decrease in
estrogen levels. Symptoms vary widely among women but commonly include mood
changes, hot flashes, vaginal dryness, and urinary incontinence.
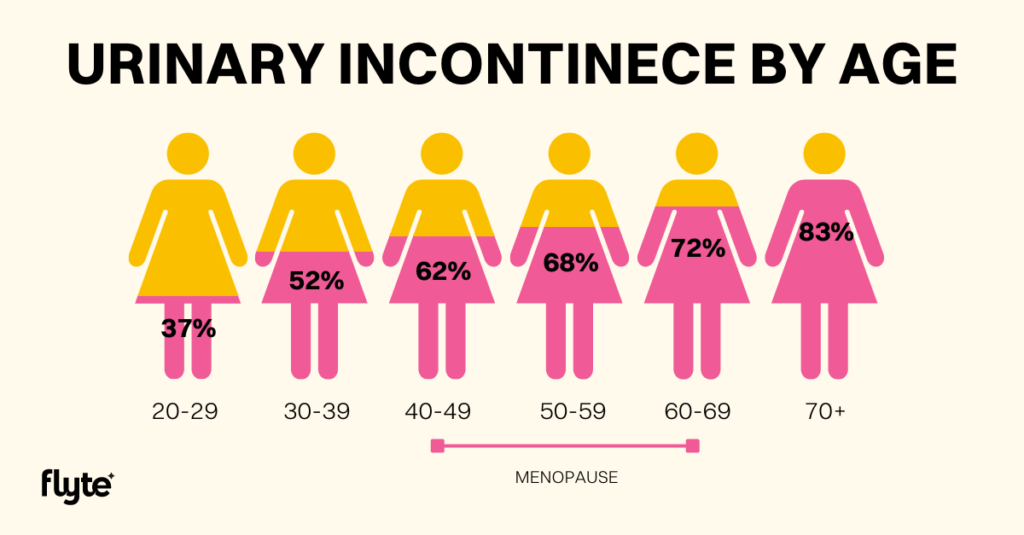
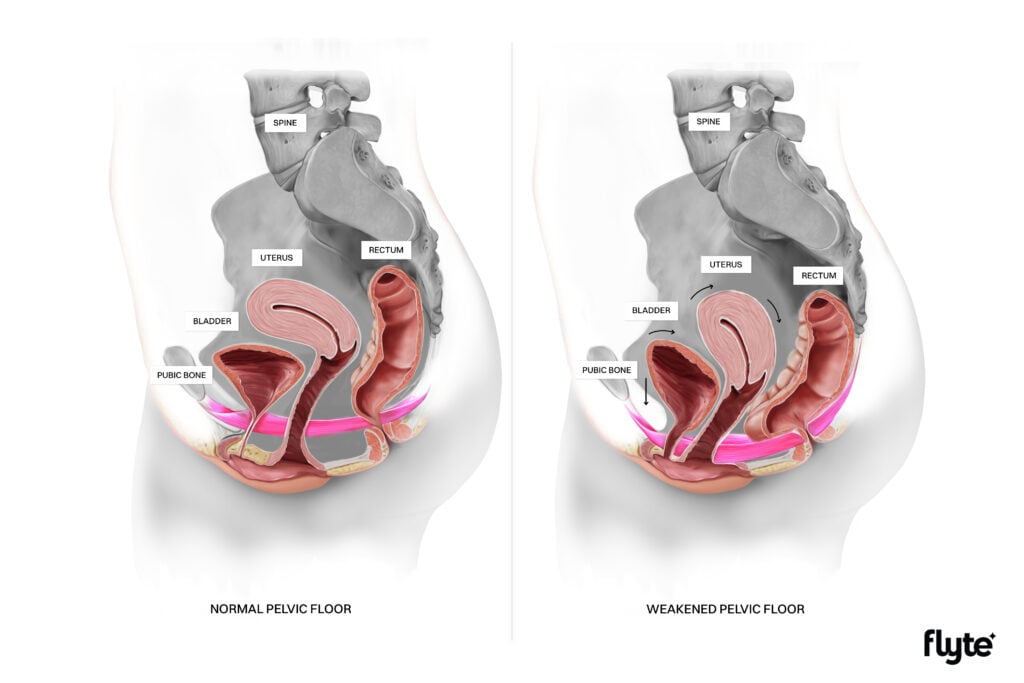
A 2022 research study reported a staggering 62% of adult women in the United States suffer from urinary incontinence and it only worsens with age. While menopause does not directly cause urinary incontinence, the hormonal fluctuations and aging processes associated with it can exacerbate or contribute to the condition. Factors such as pelvic floor muscle weakness, decreased muscle mass due to lifestyle changes, unresolved past issues, childbirth history, constipation, and decreased water intake can all play a role in the onset or worsening of urinary incontinence during menopause.
A 2024 pelvic health study surveyed 612 women ages 18-59 and examined the prevalence of pelvic health symptoms and the gaps in the care they seek and receive.
- 83% of women in this age group reported at least one pelvic health symptom in the past year and of those with symptoms, 96% say they have not been diagnosed.
- Nearly 50% of women in peri/menopause say bladder leaks started or worsened in this stage of life.
- 63% of women in peri/menopause experienced bladder leaks in the last year.
- 40% of peri/menopause women haven’t received medical care for their pelvic symptoms.
This new pelvic health study lists the barriers these women reported to getting care for menopausal symptoms including lack of education as the most common reason followed by lack of time/energy or money to prevent care.
Navigating through menopausal symptoms can feel overwhelming, especially when it seems like barriers stand in the way of getting the care you need. Educating yourself, asking your healthcare provider questions, exploring telehealth options for scheduling convenient appointments, and asking about any financial assistance programs are all options to help overcome the barriers to seeking care.
Genitourinary Syndrome of Menopause
Genitourinary Syndrome of Menopause (GSM) encompasses various changes in the vulva, vagina, and lower urinary tract resulting from decreased estrogen levels. Symptoms include vaginal dryness, reduced lubrication, pain with intercourse, and urinary issues like increased urgency, frequency, and urinary incontinence.
50-70% of postmenopausal women experience GSM. Managing GSM can include use of vaginal lubricants and vaginal moisturizers to alleviate discomfort and ease insertion, hormone replacement therapy and vaginal estrogen cream to bolster tissue health, and pelvic floor physical therapy to address muscle dysfunction and improve symptoms.
Some women worry about side effects associated with estrogen therapy. A new 2024 review study found that estrogen therapy, in addition to helping with hot flashes (vasomotor symptoms) and other menopause-related symptoms, carries little risk at increasing cancer. In fact, this new review finds estrogen therapy might decrease the risk of breast cancer, as also reported in Forbes.
Understanding Urinary Incontinence
Urinary incontinence can manifest in different forms during menopause, including stress urinary incontinence, urgency urinary incontinence, or mixed urinary incontinence as the most common.
- Stress urinary incontinence (SUI): Involuntary urine leakage, or bladder leaks, with activities like coughing or laughing, often stems from weakened pelvic floor muscles unable to adequately support the bladder and urethra. Menopause-related hormonal changes and tissues alterations can exacerbate this condition.
- Urgency urinary incontinence (UUI): A strong, uncontrolled urge to empty the bladder often leading to involuntary urine leakage. Menopause-related hormonal changes and tissues alterations can also exacerbate this condition.
- Mixed urinary incontinence (MUI), is a combination of both stress and urgency incontinence symptoms.
Despite urinary incontinence being a commonly reported symptom during perimenopause and menopause, it is not a normal or inevitable result of getting older. You do not have to accept urinary incontinence during menopause. There are effective treatments available.
Charting Your Symptoms
Charting your symptoms can help you track your symptoms and improve your communication of symptoms to your provider. From the sensation of dryness, painful vaginal insertion, urinary urgency/frequency/incontinence episodes in a day, to the numbers of pads used in a day, documenting these symptoms enables better communication with your healthcare provider and facilitates a more tailored treatment plan. Consider tracking your symptoms in a bladder diary that you can share with your provider at your next visit.
Implementing At-Home Strategies
At-home strategies play a crucial role in managing urinary incontinence during menopause.
- Increase your water intake
- While reducing water intake may seem like the intuitive solution when having a leaky bladder, it can exacerbate symptoms. Reducing your water intake causes your urine to become concentrated, irritating the lining of your bladder, and can worsen urgency, frequency, and urinary incontinence. Reducing your water intake can also lead to constipation that additionally may worsen urinary symptoms. Gradually increase your water intake (1-2 oz/day), aiming for half your body weight in ounces or approximately 64-68 ounces per day.
- Learn “The Knack”
- The Knack is a useful technique used in pelvic floor physical therapy to help with leaks associated with sneezing, coughing, laughing, etc. It is a well-timed contraction of your pelvic floor where you…
- Contract your pelvic floor muscles prior to and during the activity that causes bladder leaks
- Hold your squeeze during the activity that causes the bladder leaks
- Release your pelvic floor muscles when the activity is done
- The Knack is a useful technique used in pelvic floor physical therapy to help with leaks associated with sneezing, coughing, laughing, etc. It is a well-timed contraction of your pelvic floor where you…
- Diaphragmatic breathing
- Learning to breathe with your diaphragm helps to improve the function of your pelvic floor muscles. During diaphragmatic breathing, your belly, not only your chest, expands in the front, sides, and back while inhaling and relaxes while exhaling. This technique helps to manage intra-abdominal pressure and urinary incontinence.
Exploring Treatment Options
Several treatment options exist for managing urinary incontinence during menopause. You can talk with your healthcare provider about treatment options available for you that may include pelvic floor strengthening, using an at-home pelvic floor device, various medications, or other more invasive treatment options, including surgery.
Embracing Menopause with Confidence
Women can reclaim control over their menopause symptoms by speaking up and refusing to accept that they must live with menopause-related symptoms or by being dismissed by healthcare providers. Being proactive about seeking solutions, including through telehealth, and by having a strong support system can make a significant difference in managing menopause-related symptoms and improving overall health.
Menopause, despite its challenges, represents a transformative phase in a women’s life. By leveraging and advocating for available treatment options, adopting self-care practices, and seeking support from healthcare professionals, women can confidently live and thrive in this new phase of life.
Sponsored by Flyte.

This blog article was authored and reviewed by pelvic floor physical therapists Leah Fulker, PT, DPT, PCES and Shravya Kovela, PT, DPT, OCS.
Pelvic floor muscle strengthening with Flyte can stop or reduce bladder leaks. Flyte® is an FDA-cleared at-home treatment for bladder leaks. Flyte uses the proven treatment modality of mechanotherapy to strengthen and tone the pelvic floor muscles in only 5 minutes a day for 6 weeks. In clinical trial, 82% of women were continent in 6 weeks. Flyte’s mechanotherapy was shown in research to increase the impact of your Kegels by 39x – meaning you see results quickly. Flyte is a convenient, easy, and effective treatment solution for women seeking relief from bladder leaks with results comparable to surgery in a non-invasive treatment option from the comfort of home.






2 Responses
Does reduced water intake affect urinary incontinence in men too . And how does Pelvic floor strength affect sex
In 2022 I was diagnosed with ER PR Positive Breast Cancer. I had been on ERT Eztrogen only since I had my uterus and ovaries removed in 1992. I was on the lowest dose patch. I had to stop the patch. At the same time I got Covid and the worst UTI of my life. I have been to 3 different Urologists. My Urge Incontinence got worse. My bladder is so sensitive. I just has a CT scan to see if there was anything else going on. I was told I had Covid Bladder. I think I still have that. Incontinence occurs mostly at night. I have hot flashes and cold flashes are in tge cold weather. Miserable. I don’t feel well then. Tge radiation treatments damaged the tendons in my right arm. Tge Oncokogist wanted me to take Tamoxifen and I refused. Too many side effects. My Estrogen level is negligible.