BOTOX® For Overactive Bladder
JOIN OUR NEWSLETTER
Receive custom tools to help you manage your condition and get the latest in bladder and bowel health from NAFC!
What Is Botox®?
Botox® isn’t just for wrinkles—it’s also a proven treatment for overactive bladder (OAB). If you’ve been struggling with leaking, strong sudden urges to go, or going too often—even after trying pills—Botox® for urinary incontinence may help.
Botox® is a prescription medicine injected into the bladder muscle. It helps calm the nerves that cause OAB symptoms so your bladder doesn’t squeeze when it shouldn’t.
How Does Botox® For Overactive Bladder work?
With OAB, nerves tell your bladder to contract—even when it’s not full. That’s what causes sudden urges and leaks.
Botox® works by blocking these extra signals from the nerves to the bladder muscle. When the signals stop, your bladder relaxes—and you get fewer leaks and bathroom trips.
In clinical trials:
- People had an average of 3 fewer leaks per day with Botox® (vs. just 1 fewer with a placebo).
- About 1 in 4 people had their leakage stop completely.
- Most people needed just 2 treatments a year.
Is Botox® Right For Me?
Botox® might be a good option if:
- You’re looking for a way to significantly reduce daily leakage episodes.
- You’ve tried OAB pills, but they didn’t work or had bad side effects.
- You’re tired of planning your life around the nearest bathroom.
- You want a treatment that works for up to 6 months at a time.
The decision to use BOTOX® should be one that you and your doctor decide on together. Talk with your doctor if you’re unsure. Together, you can determine if BOTOX is an option for you.
Download a doctor discussion guide to help you navigate the conversation about Botox.
Kristie's Story: My Search For An Effective OAB Treatment
What To Expect At Your Appointment
Botox® is given in the comfort and convenience of your doctor’s office and takes about an hour from start to finish. Here’s what happens:
Before the visit:
- Your doctor will prepare for your appointment by completing any necessary paperwork and ensuring all the details are handled for a seamless treatment experience.
- You’ll be prescribed antibiotics to help prevent a urinary tract infection. These should be taken before, on, and after the day of treatment.
During the visit:
- Your bladder will be numbed with a local anesthetic. This process takes roughly 20 minutes.
- The doctor will place the Botox® in the bladder muscle. The procedure takes about 10 minutes.
- You’ll stay for about 30 minutes after the injection to make sure you’re doing well.
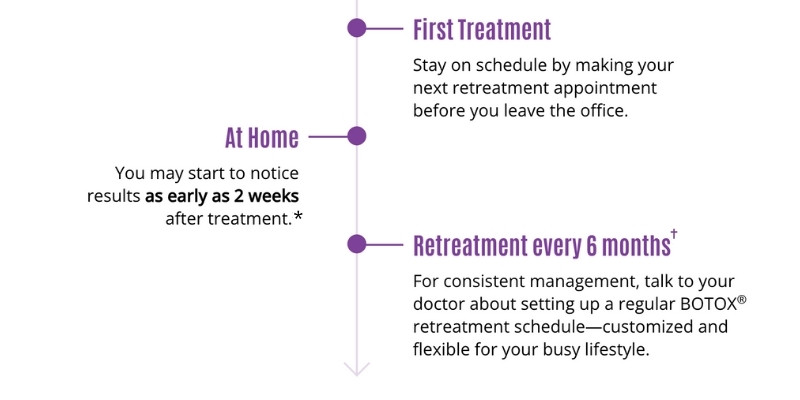
- You’ll schedule your re-treatment for 6 prior to leaving your doctors office.
After the visit:
- You might feel a little burning when you pee for the first day or two.
- Results can start in as little as 2 weeks.
- The treatment can last up to 6 months, and then you can come back for a retreatment.
Kristie's Story: My Botox Procedure Experience
Why It's Important To Stay On Treatment
OAB is a long-term condition. Just like with other health conditions, staying on a regular treatment schedule helps you feel your best.
Talk to your doctor about setting up reminders and make sure to book your next appointment before you leave the office.
Kristie's Story: Why I Come Back Regularly For Re-treatment
How Can I Save Money On Botox Treatments?
Most people with insurance, including Medicare, have coverage for Botox® for OAB. And if you have commercial insurance, you may be eligible for the BOTOX® Savings Program.
You could pay as little as $0 out of pocket.*
Kristie's Story: How To Save Money On BOTOX for OAB
Want To Find A Specialist?
If you’re ready to explore Botox® for urinary incontinence, use this tool to find a provider near you.
Still Have Questions?
Talk with your doctor or visit https://www.botoxoveractivebladder.com/botox-for-oab to learn more.
Related Articles

Acupuncture and Chinese Herbs for the Benefit of OAB
Traditional Chinese medicine (TCM) has been treating urinary symptoms such as overactive bladder for more than 2,000 years. Acupuncture and Chinese medicinal herbs potentially offer

How I Survive Traveling With Incontinence (and Three Kids)
I’ve never been one of those moms who can fly by the seat of her pants and wing it. Especially when traveling. A mother of

Ask The Doc: Insurance Coverage For Pelvic Floor Strengthener
Leva explains how to get insurance coverage for pelvic floor strengtheners

8 Most Common Questions About Fistulas – Answered!
If you’ve been diagnosed with a fistula, you may have some questions about what it is, why you have it, and what can be done.